- Folded Ear in Newborns: Treatment Options - April 11, 2018
- Newborn Ear Deformity: What Can Be Done? - April 11, 2018
- Ear Molding: An Overview - November 2, 2017
- Otoplasty for Protruding Ears - September 26, 2017
- Basal Cell Carcinoma: Facial Reconstruction Timing - September 26, 2017
- Clinical Considerations of Mohs Reconstruction of Cheek Defect - September 26, 2017
- Basal Cell Carcinoma: Nasal Bridge Reconstruction - September 26, 2017
- Skin Cancers Involving the Eyebrow: Clinical Considerations - October 3, 2016
- Treatment of Multiple Skin Cancer Lesions - June 1, 2016
- Skin Cancer: Nasal Reconstruction and Scar Management - June 1, 2016
- India Medical Mission 2018 - November 1, 2018
- Sleep Disorders: Sleep Apnea and Upper Stimulation Therapy - August 25, 2015
- The Naked Vocalist Podcast Featuring Dr. Reena Gupta - May 27, 2015
- New Therapy for Sleep Apnea – First Sleep Pacemaker placed in California at Osborne Head and Neck Institute. - December 12, 2014
- Boxer’s Ear: Can your ear explode? - December 12, 2014
- Nose Picking (Rhinotillexis) and Septal Perforations: Why I should stop picking my nose…? - November 24, 2014
- Deviated Septum and Septal Perforation - July 28, 2014
- Hereditary Hemorrhagic Telangiectasia: Nasal Septal Perforation Repair - June 25, 2014
- Dr. Mantle recognized at the Beverly Hills Medical Science Academy Awards - May 8, 2014
- Commonly Misdiagnosed Pathologies: Arteriovenous Malformations - April 9, 2014
Question: I’m having skin cancer removed from my nose. How long should I expect to have before my scar is noticeable?
Case Study
The patient is a male in his 50s who noticed a small bump growing over the tip of his nose for a few months. He presented to his dermatologist who took a biopsy of his lesion. The biopsy was positive for basal cell carcinoma (BCC). The patient presented to a Mohs surgeon for excision of this lesion and followed up with Dr. Zandifar for nasal reconstruction. The nasal tip defect was reconstructed with a local rotational flap. After surgery the scar was treated with Intense Pulse Light (IPL) for 3 sessions. The patient was instructed to apply a silicone-based gel with sunscreen to the scar. Three months after reconstruction the scar is hardly noticeable and patient is extremely happy with the outcome.
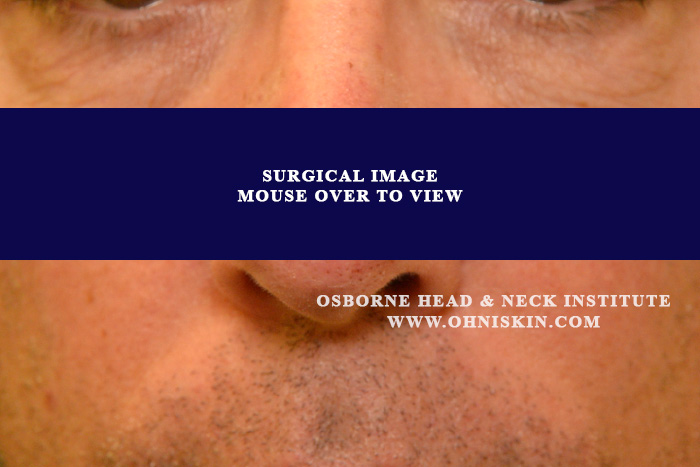
Figure 1: The defect after excision by Mohs surgeon.

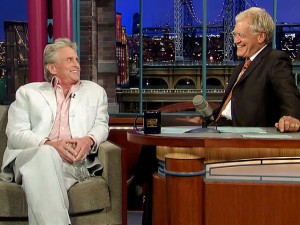
Figure 2: The defect 3 months after reconstruction by Dr. Zandifar.
Discussion
Basal cell and squamous cell skin cancers are the most prevalent types of cancer worldwide. Approximately 85% of all of these skin cancers arise in the head and neck region. The nose is a common site of presentation for these types of skin cancer because of its prominent position on the face.
After excision of a skin cancer lesion, the resulting defect and the healing scar can be readily visible. Consequently, proper reconstruction of a resulting defect becomes extremely important for both functional and cosmetic reasons. In order to obtain a cosmetically appeasing result, post-operative care of the wound also becomes an important factor.
Use of post-operative therapies such as lasers and light therapy can facilitate healing and improve the overall appearance of a scar. Application of silicone-based gels to the surface of a scar is also an effective option. The combination of these two techniques promotes the healing process and ultimately can improve the overall cosmetic look of a healing scar. In order to achieve an optimal result, a reconstructive surgeon should utilize techniques that promote optimal functional and cosmetic results as well as encourage appropriate post-operative care.
The physicians of the Osborne Head and Neck Institute are board certified in otolaryngology and facial plastic and reconstructive surgery. This combination of specialties allows the physicians of OHNI to customize procedures and treatment plans for patients that promote optimal results all around.
To learn more about Dr. Hootan Zandifar or reconstruction following skin cancer, please visit: www.ohniskin.com.