- Graves’ Disease: General Overview - September 25, 2017
- The Effect of Bulimia on the Parotid Gland - September 25, 2017
- Graves’ Disease: Treatment Overview - September 25, 2017
- India Medical Mission 2018 - November 1, 2018
- Sleep Disorders: Sleep Apnea and Upper Stimulation Therapy - August 25, 2015
- The Naked Vocalist Podcast Featuring Dr. Reena Gupta - May 27, 2015
- New Therapy for Sleep Apnea – First Sleep Pacemaker placed in California at Osborne Head and Neck Institute. - December 12, 2014
- Boxer’s Ear: Can your ear explode? - December 12, 2014
- Nose Picking (Rhinotillexis) and Septal Perforations: Why I should stop picking my nose…? - November 24, 2014
- Deviated Septum and Septal Perforation - July 28, 2014
- Hereditary Hemorrhagic Telangiectasia: Nasal Septal Perforation Repair - June 25, 2014
- Dr. Mantle recognized at the Beverly Hills Medical Science Academy Awards - May 8, 2014
- Commonly Misdiagnosed Pathologies: Arteriovenous Malformations - April 9, 2014
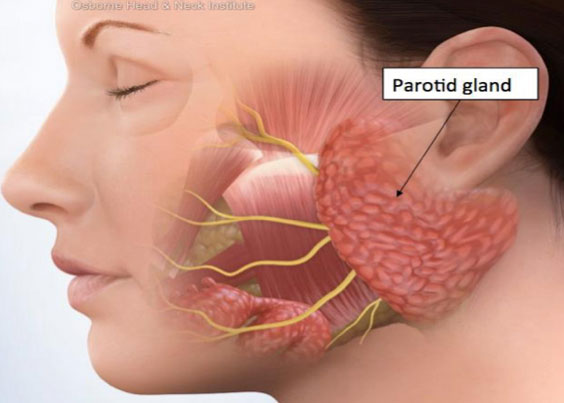
The parotid gland is the largest of three salivary glands in the human body and is partly responsible for the production of saliva which contains enzymes that function to lubricate the digestive tract and assist in breaking down and swallowing food. There is one gland located in each cheek sitting above the jaw and beside the ear. The glands are adversely affected by chronic vomiting that occurs in patients with bulimia.
Bulimia nervosa is an eating disorder in which patients go through periods of binge eating and purging. It is characterized by a chronic cycle that begins with a compulsive urge to overeat followed by extreme feelings of guilt and regret that ultimately drive the individual to induce vomiting. The disease can affect men and women as young as 8 years old but is most common in females starting at the age of 14. It results in a multitude of damaging effects on the body, in particular, the digestive system.
When gastric acid from the stomach is constantly passing through the digestive tract in the wrong direction, it greatly damages tissues lining the esophagus and mouth. When the body is preparing to vomit, the salivary glands increase production of saliva to lubricate the esophagus and mouth in an effort to protect the tissues from the acidity of the vomit. Because patients with bulimia typically induce vomiting multiple times a day, they are forced to produce excess amounts of saliva which causes their parotid salivary glands to become over-stimulated. In order to keep up with the amount of work that is being asked of them, the glands increase in size which is defined as parotid hypertrophy.
Parotid hypertrophy is commonly misdiagnosed as parotitis. Parotitis is defined as inflammation of the parotid glands and can be caused by a number of things. It cannot, however, occur as a direct result of bulimia because the chronic exposure to vomit does not inflame the glands but rather causes them to increase in size, or become hypertrophic. The reason this is so commonly misdiagnosed is because when patients observe the physical effect the hypertrophic glands have on their face, “enlarged cheeks,” they associate the enlargement with the word, “inflammation.” It can also be difficult for physicians to discover the connection between the hypertrophic glands and the bulimia because patients with the eating disorder are often times very secretive and/or in denial.
Parotid hypertrophy itself is not dangerous. It is, however, crucial to treat the underlying issue of bulimia. The body is not able to sustain the damage caused by the disease and eventually dehydration and malnutrition cause complications in different organ systems. It is ultimately fatal if not treated. Treating bulimia generally involves a form of therapy and an antidepressant and/or anxiety medication.
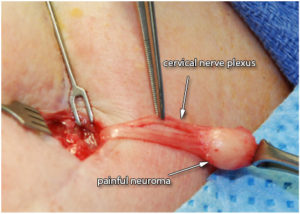
After a prolonged period of regular eating, the parotid glands will most likely return to their original state. Once they are no longer required to produce excessive amounts of saliva, they are able to adapt and shrink. In the rare case that the glands do not reduce in size after an extended period without purging, the only other treatment option is to surgically remove a portion of the gland through a total superficial parotidectomy. The parotid glands are divided into two lobes, deep and superficial. Removing the superficial lobe slims the face, allowing for a more cosmetically appealing look. However, patients may be reluctant to have surgery because traditional procedures can lead to visible scars on the side of the neck. This concern can be especially pertinent in bulimic patients who tend to struggle with self-image. In addition, the complication of the facial nerve discourages many from having the surgery due to the risk of facial paralysis.
The facial nerve is the seventh cranial nerve and is responsible for controlling the muscle movement in the face as well as taste and feeling in the ear. The nerve passes through the gland and demarcates the barrier between the deep and superficial lobes. Within the gland, the nerve divides into 5 branches and each branch then divides into smaller branches. Each must be located and individually dissected in order to remove the superficial lobe without damaging the nerve and therefore causing facial muscle weakness or paralysis.
The Osborne Head and Neck Institute routinely performs parotidectomy procedures and has a 100% success rate without any occurrence of facial paralysis. For some, however, these concerns outweigh the benefits of surgery. There are risks involved in any procedure and living with parotid hypertrophy is not dangerous. For others, the surgery provides relief from a constant reminder of their past obstacles.
Key Points
- The parotid glands are salivary glands located in the cheeks that produce saliva to lubricate the digestive
- Bulimia nervosa is an eating disorder characterized by binge eating and purging that greatly damages the digestive
- The parotid glands become hypertrophic in people with bulimia because they produce excess saliva to protect the esophagus and mouth from the acidic
- Parotid hypertrophy is commonly misdiagnosed as
- Hypertrophic glands generally return to normal size once the bulimia is treated and regular eating habits
- Total superficial parotidectomies remove the superficial lobe of the parotid gland to create a more cosmetically appealing
- Surgical complications include facial paralysis and It is recommended that these procedures be performed by specialized and experienced surgeons.
To learn more about parotid hypertrophy or parotidectomy, please visit: www.ohni.org.