- Cranial Nerves: An Overview - September 25, 2017
- Skin Cancer: An Overview - September 25, 2017
- Shingles and Facial Nerve Damage - May 1, 2014
- Tattoo Removal - October 23, 2013
- Folliculitis: Frequently Asked Questions - April 12, 2011
- Adenoids: Frequently Asked Questions - April 12, 2011
- Serum Injection - September 17, 2010
- Treatment of Acne and Rosacea - September 10, 2010
What Are Cranial Nerves?
Cranial nerves are the nerves that directly originate from the brain or brainstem. They are primarily responsible for transmitting impulses and information from the brain to regions in the head and neck. There are 12 pairs of cranial nerves that are either sensory, motor, special (taste and smell), or mixed (both sensory and motor). Various injuries or illnesses can negatively affect the cranial nerves and lead to a number of adverse conditions known as cranial neuropathies. The type of neuropathy is dependent upon which of the cranial nerves is affected.
Olfactory Nerve (CN I)
The olfactory nerve is responsible for providing the sense of smell. It is a sensory nerve that ends in the upper part of the nasal cavity. This cranial nerve is the shortest of the 12 nerve pairs and is unusual in that it is capable of undergoing some regeneration if damaged. The process of interpreting odors begins when small particles with varying properties enter the nasal cavity and stimulate the receptors on the olfactory nerve. This stimulation is transformed into electrical activity that is then transmitted to the brain.
If the olfactory nerve is damaged, the possible neuropathies are either anosmia (the complete inability to smell) or dysosmia (a distortion in the sense of smell). Such damage may be caused by brain injury or using certain types of nasal spray. To confirm that the ability to smell is affected, both nostrils are usually tested with substances of known smells such as apples, coffee, or soap.
Optic Nerve (CN II)
The optic nerve is responsible for conveying the sense of sight. It is a sensory nerve that connects the retina to the brain. The retina receives all of the light that enters the eye and sends the visual information (brightness, color, etc.) to the brain via the optic nerve. This nerve is also responsible for the accommodation reflex in which the eye adjusts according to the distance of the object in focus.
The most common cause of optic neuropathy is poor blood flow that can be the result of various health issues such as diabetes, obesity, and heart conditions. Additional causes include trauma, exposure to radiation/toxins, and shock. Initial symptoms of this damage include a reduced field of vision (bitemporal hemianopsia), fading of colors, and an inability to see fine detail. This damage cannot be reversed, so the underlying cause must be treated to prevent further deterioration of vision.
Oculomotor (CN III), Trochlear (CN IV), and Abducens (CN VI) Nerves
The oculomotor nerve (CN III), trochlear nerve (CN IV), and abducens nerve (CN VI) are motor nerves responsible for coordinating eye movement. Damage to these nerves affects the movement of the eyeball (either one or both) and in most cases, causes double vision (diplopia). The function of these nerves is usually tested by moving a small object in front of the eyes and seeing how they follow it.
The oculomotor nerve innervates the muscles that are responsible for the majority of the movements of the eye. It also coordinates movement of the eyelid. If this nerve is damaged, numerous conditions could arise including diplopia, desynchronization of eye movements (strabismus), drooping of the eyelids (ptosis), and dilation of the pupils (mydriasis).
The trochlear nerve controls an eye muscle that is responsible for two movements: downwards (depression) and toward the nose (intorsion). Damage to this nerve results in a diplopia in which the eye cannot properly move downwards.
The abducens nerve also controls just a single muscle that is responsible for the lateral movement of the eye. Like the other two nerves, damage to this nerve usually results in diplopia.
Trigeminal nerve (CN V)
The trigeminal nerve is responsible for providing sensation to the face and innervating the muscles responsible for chewing and biting. It is the largest of the cranial nerves and is composed of three branches: the ophthalmic (V1), maxillary (V2), and mandibular (V3) nerves. The first two branches are sensory nerves while the mandibular branch has both sensory and motor functions (mixed).
Trigeminal neuralgia is the main condition that affects the trigeminal nerve, but cluster headaches and trigeminal zoster (facial rashes) can also occur. Trigeminal neuralgia is often described as the most painful human condition as it causes severe pain with a burning or stabbing sensation. As with other nerves, this type of neuralgia is usually caused by the compression of the nerve root by blood vessels or by physical damage to the nerve.
Facial nerve (CN VII)
The facial nerve controls the muscles responsible for facial expression and conveys the sense of taste. It receives taste sensation from the front ⅔ of the tongue through one of its branches known as the chorda tympani. In addition to controlling the muscles of facial expression, the facial nerve also innervates the stapedius muscle located in the middle ear which is responsible for protecting our ears from loud noises.
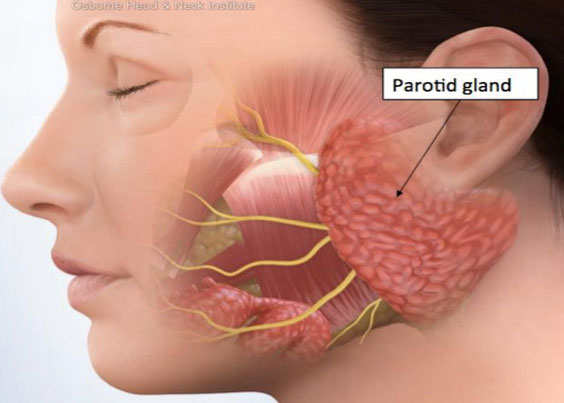
Damage to the facial nerve may result in facial palsy, a condition in which a person is unable to move certain facial muscles. Bell’s palsy is a common, and usually temporary, facial palsy characterized by the inability to move one side of the face. Individuals with Bell’s palsy often cannot elevate their eyebrow or furrow their forehead on the affected side.
Vestibulocochlear nerve (CN VIII)
The vestibulocochlear nerve, which splits into the vestibular and cochlear branches, connects the inner ear to the brain and is responsible for providing sensory information regarding balance and hearing to the brain. The vestibular nerve innervates the vestibule and semicircular canals which together transmit information about balance. The cochlear nerve terminates at the cochlea where it receives electrical impulses relating to sound.
Damage to the vestibular branch can cause sensations of dizziness and spinning. When the cochlear branch is damaged, the affected ear will exhibit complete deafness or severe hearing loss.
Glossopharyngeal nerve (CN IX)
The glossopharyngeal nerve is a mixed nerve that receives taste sensations from the back ⅓ of the tongue and controls some muscles responsible for swallowing. It also innervates the tonsils and pharynx from which it receives sensory information. Lesions of this nerve could often cause an absence of a gag reflex. Damage could also lead to impaired swallowing and, in some cases, the loss of bitter and sour taste.
Vagus nerve (CN X)
The vagus nerve is the longest nerve of the parasympathetic nervous system, the system responsible for our body’s unconscious actions. It is a mixed nerve that provides parasympathetic innervation for all of the organs and is thus responsible for regulating heart rate, sweating, peristalsis, and a significant amount of muscles in the mouth (including speech since it innervates the larynx via the recurrent laryngeal nerve).
Damage to the vagus nerve could lead to a rise in blood pressure and heart rate as well as difficulty swallowing. Issues with the vagus nerve can often be diagnosed from a hoarse voice which would stem from dysfunction of the recurrent laryngeal nerve.
Spinal accessory nerve (CN XI)
The spinal accessory nerve is a motor nerve that innervates the sternocleidomastoid and trapezius muscles. The sternocleidomastoid muscles are responsible for turning the head while the trapezius muscles control the action of elevating the shoulders.
Damage to this nerve generally results in weakness of the sternocleidomastoid and trapezius muscles. The patients would have difficulty raising their shoulders or turning their heads.
Hypoglossal nerve (CN XII)
The hypoglossal nerve is a motor nerve that innervates all the muscles of the tongue and is thus responsible for tongue movement. It controls certain movements required for swallowing and speech, such as sticking out the tongue and moving it left and right.
Damage to this nerve can arise from compression by tumors or from an injury caused by trauma or surgery. Hypoglossal nerve damage can impact the tongue’s ability to move and affect its appearance. Lesions usually lead to tongue weakness on one side. In cases like this, the tongue can be observed to move asymmetrically towards the affected side.
To learn more about the cranial nerves such as the facial nerve, please visit: www.ohni.org/.