- Question: How do the ingredients in e-cigarettes and vaporizers affect respiratory health? - August 16, 2019
- Bad Technique and Vocal Injury - January 9, 2019
- Is Edible Marijuana Dangerous for the Voice? Myths Dispelled - December 18, 2018
- Surprise! You have a hemorrhage - January 31, 2018
- Graves’ Disease: Treatment Overview - September 25, 2017
- Adele and the Stigma of Vocal Injury - July 11, 2017
- Vocal Curbside Consult: How does the thyroid affect the voice? - May 16, 2017
- Vocal Curbside Consult: How do hormones affect the voice? - May 3, 2017
- Vocal Curbside Consult: How do emotion and stress affect the voice? - April 17, 2017
- Vocal Curbside Consult: Vocal Recovery After Illness - April 7, 2017
 Meghan Trainor, talented songwriter and singer, has had to stop performing and cancel the remainder of her tour due to a second vocal hemorrhage. Singers, vocal coaches, and fans have been scratching their heads over this injury, as hemorrhages have not been discussed much in the vocal community. Nodules, thick vocal fold callouses, are the most feared diagnoses among singers. What they have not yet been taught is that the hemorrhage is the original insult and should be the real focus of our attention.
Meghan Trainor, talented songwriter and singer, has had to stop performing and cancel the remainder of her tour due to a second vocal hemorrhage. Singers, vocal coaches, and fans have been scratching their heads over this injury, as hemorrhages have not been discussed much in the vocal community. Nodules, thick vocal fold callouses, are the most feared diagnoses among singers. What they have not yet been taught is that the hemorrhage is the original insult and should be the real focus of our attention.
It used to be that singers would “push through” injuries, singing while sick and accepting hoarseness as a badge of honor or a necessary evil after a performance. Teas, lozenges, scarves, and steroid shots were Band-Aids that allowed the singer to push through the next day again. When pushing became impossible for them, they would seek attention. At this point, they often received the diagnosis of nodules and this reviled pathology became common and feared.
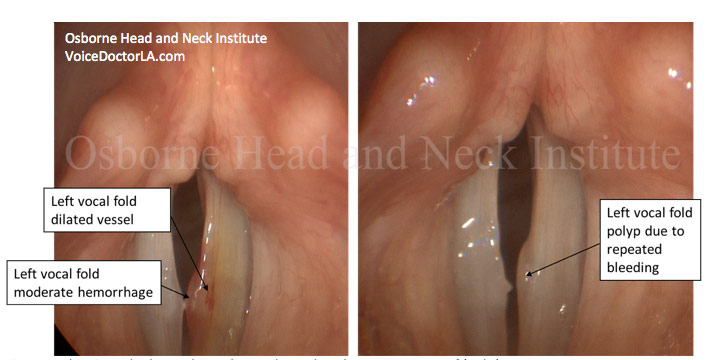
We have come to understand more about nodules and vocal injury, specifically how injuries form. When the voice is pushed past its natural limits, the vocal folds may bruise.
Vocal demands are extremely high on the touring performer. When high demand is compounded by even a small issue like a cold, this will often precipitate a hemorrhage.
Small blood vessels in the vocal fold burst which results in blood leaking into the vocal fold. There may be a small amount of blood, resulting in hoarseness that the singer feels they can “work around.” The voice change from a small hemorrhage is only slight, and so it is common for the singer to ignore it and proceed with singing.
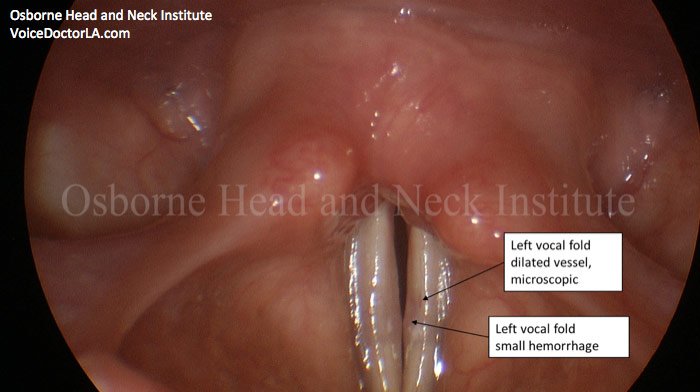
The small hemorrhages are the dangerous ones. Unknown to the singer, they are pushing through an injury which, due to continued voice use, allows inflammation and scarring to develop. After repeated hemorrhagic injury, this will become nodules (or a polyp, or a cyst, or any other vocal injury) if left undiagnosed. The “push” past small hemorrhages is the problem that leads to eventual larger problems.
Mirrors in the mouth or flexible scopes in the nose are still used by many ENTs to screen the vocal folds. These exams miss small hemorrhages, giving performers who have these exams a false sense of security when they are evaluated and told they are fine. The “steroid shot and send them on their way” approach misses small, early injuries that evolve into bigger injuries. The singer will only get a diagnosis when the injury is large enough for these technologies to catch. It is why it seems these things come out of the blue.
We, as voice professionals, need to be proactive and no longer accept inadequate training and equipment from our voice team. Other articles on this site have discussed the keys to good diagnostics in singers. In brief, singers require:
- A board-certified, fellowship-trained laryngologist; being a “voice doctor” is not enough; look for the credentials
- A fellowship-trained vocal therapist (speech pathologist with vocal injury and rehabilitation training)
- A voice team: a laryngologist, a vocal therapist, and a vocal coach
- Videostroboscopy: a rigid camera inserted into the mouth. Mirrors in the mouth and flexible scopes in the nose are inadequate to find early injury
- A close follow up plan for the high-intensity performer. Steroids alone are a set-up for further injury when there is no larger, long-term plan
- A screening exam (videostroboscopy) when healthy and vocal therapy when demand is high, before injury has occurred.
To learn more about Dr. Reena Gupta or voice evaluation and treatment, please visit www.voicedoctorla.com.
Image Credit: Meghan Trainor – By Ronald Woan from Redmond, WA, USA [CC BY-SA 2.0
(http://creativecommons.org/licenses/by-sa/2.0)], via Wikimedia Commons.



