- Hereditary Hemorrhagic Telangiectasia - May 25, 2016
- Hereditary Hemorrhagic Telangiectasia: Septal Perforation and Nose Bleeds - May 23, 2016
- Hereditary Hemorrhagic Telangiectasia: Epistaxis and Septal Perforation - May 18, 2016
- Wegener’s Granulomatosis: Autoimmune Disease and Multi-Focal Septal Perforation - May 9, 2016
- Kyle Korver: Facial Injury and Nasal Fracture - March 24, 2015
- Russell Westbrook: Facial Injury and Surgery - March 5, 2015
- Mega-perforation: Pushing the Limits of Septal Perforation Repair - November 26, 2014
- Septoplasty Complication and Septal Perforation - November 24, 2014
- Nose Picking (Rhinotillexis) and Septal Perforations: Why I should stop picking my nose…? - November 24, 2014
- Nasal Fractures, Septal Hematoma, and Septal Perforation: Simultaneous Rhinoplasty and Septal Perforation Repair - October 1, 2014
- India Medical Mission 2018 - November 1, 2018
- Sleep Disorders: Sleep Apnea and Upper Stimulation Therapy - August 25, 2015
- The Naked Vocalist Podcast Featuring Dr. Reena Gupta - May 27, 2015
- New Therapy for Sleep Apnea – First Sleep Pacemaker placed in California at Osborne Head and Neck Institute. - December 12, 2014
- Boxer’s Ear: Can your ear explode? - December 12, 2014
- Nose Picking (Rhinotillexis) and Septal Perforations: Why I should stop picking my nose…? - November 24, 2014
- Deviated Septum and Septal Perforation - July 28, 2014
- Hereditary Hemorrhagic Telangiectasia: Nasal Septal Perforation Repair - June 25, 2014
- Dr. Mantle recognized at the Beverly Hills Medical Science Academy Awards - May 8, 2014
- Commonly Misdiagnosed Pathologies: Arteriovenous Malformations - April 9, 2014
Achieving Successful Septal Perforation Repair
Background
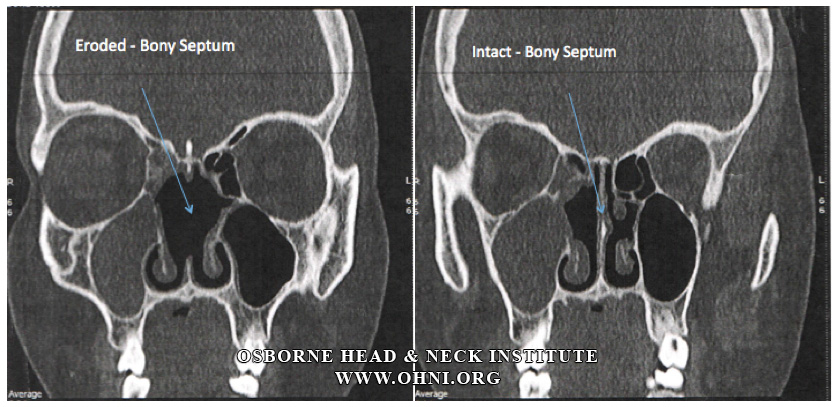
Autoimmune disorders are characterized by autoantibodies directed against the patient’s body instead of external pathogens (i.e. viruses, bacteria, etc.). In Wegener’s granulomatosis autoantibodies attack small blood vessels throughout the body, causing swelling and ultimately small inflammatory nodules called granulomas. Granulomas slow blood flow and eventually cut off vital oxygen and nutrients to affected organs causing necrosis (cell death). Small vessels within the nasal cartilage framework are particularly at risk.
Clinical Manifestations
Patients typically present with complaints of increasing nosebleeds and eventually, multiple septal perforations and nasal deformity caused by external cartilage collapse due to poor blood flow.
Medical Considerations
A Rheumatologist should evaluate all patients with a history of Wegener’s’ granulomatosis who are considering repair of a septal perforations and nasal reconstruction. Patients should be placed on appropriate immunotherapy and the disease should be successfully suppressed before any attempt at reconstructive surgery is made. Co-management with a rheumatologist is crucial.
Surgical Considerations
Successful reconstruction of any part of the body involves removing old scarred tissue and recruiting healthy tissue to rebuild the target area. In patients with Wegener’s granulomatosis, the entire septal mucosal lining may have compromised blood flow, and not be healthy enough to use for recruitment and reconstruction of a septal perforation defect. This means that the tissue around the perforation is also affected by Wegener’s disease and is unlikely able to tolerate manipulation. These cases typically require a special reconstructive technique. Reconstructive flaps based on the septum mucosal tissue should be avoided to increase the probability of successful closure and healing.
Surgeon Comments
Dr. Hamilton- “Surgeons choosing to tackle difficult septal perforation cases must have more than one choice technique that they are confortable with performing. Every case has to be approached uniquely and one technique can’t be “stretched” to cover all cases. We have developed new techniques in our practice because it is required to successfully treat a variety of cases. Accordingly, we have been able to achieve a 99% success rate for patients suffering from septal perforations using a customized surgical plan that varies for each patient. Every patient gets his or her own unique procedure.” Read patient reviews.
Dr. Jason Hamilton is the Director of Plastic and Reconstructive Surgery for the Osborne Head and Neck Institute, and is double board certified by the American Board of Facial Plastic and Reconstructive Surgery and the American Board of Otolaryngology/Head and Neck Surgery. Dr. Hamilton is one of only handful of septal perforation specialist worldwide.
For more information on the deviated septum, septoplasty, functional rhinoplasty and septal perforation repair by Dr. Jason Hamilton, septal perforation specialist, please contact the Osborne Head and Neck Institute or visit www.perforatedseptum.com.