- What is Vocal Cord Paralysis? - December 15, 2015
- Have You Heard of Wegener’s? - December 15, 2015
- Otitis Externa – Swimmer’s Ear - December 15, 2015

- Risks of Surgery for Surfer’s Ear - October 26, 2017
- The Dangers of Untreated Exostosis / Surfer’s Ear - October 26, 2017
- Surfer’s Ear Treatment: Chisel vs Drill - October 26, 2017
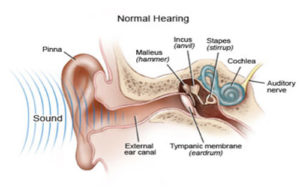
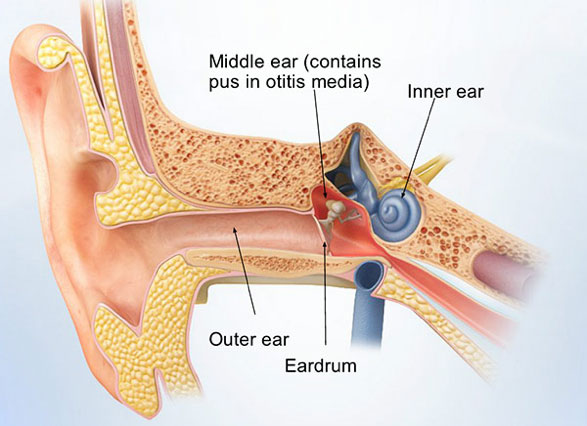
Otitis externa is inflammation of the external ear canal. Otitis externa has many possible causes:
- Bacterial: Bacteria can infect the outer ear when the skin is damaged.
- Moisture in the ear (from swimming, showering, or other aquatic-related activities) along with the body’s natural heat creates an optimal environment for bacteria to grow; this is commonly also referred to as swimmer’s ear.
- Ear trauma: This includes cleaning the ear (i.e., Q-tips)
- Eczema: This skin condition causes the skin to become inflamed and itchy.
Otitis externa can vary considerably in both severity and duration. Symptoms, therefore, also vary according to the severity of disease. People with otitis externa will often have some of the following symptoms:
- Hearing loss
- Itching
- Fluid discharge
- Feeling of fullness in the ear
- Redness in the ear
- Fever
- Tinnitus
There are three major categories of otitis externa:
Acute Otitis Externa (AOE): Acute otitis externa is recent in onset. These patients’ symptoms typically begin with a sensation of pain and itchiness in their ear(s). At this stage, OE can be treated fairly quickly.
Chronic Otitis Externa (COE): If left untreated, or treated improperly, AOE will persist and become chronic otitis externa. Symptoms are more significant and will take longer to treat.
Fungal Otitis Externa: Fungal otitis externa is often caused by overuse of antibiotics. The skin of the ear canal can become over colonized with fungal species that appear white (hyphae).
Necrotizing Otitis Externa: Although quite rare, necrotizing otitis externa is the most severe classification of this condition and is typically seen in immunocompromised patients. Necrotizing otitis externa destroys the tissues of the ear as it penetrates deeper into the skin. It can lead to sequela such as facial nerve paralysis, cranial nerve injury, meningitis, or other life threatening complications. Suspected cases of necrotizing otitis externa should be reported to an otolaryngologist immediately.

An otolaryngologist (ENT) will usually be able to diagnose otitis externa based on the symptoms themselves. The doctor will examine the ear canal and eardrum using a simple, painless examination called otoscopy. If the patient is immunocompromised or at increased risk of a fungal infection, the doctor will perform a special test called a gram stain to detect the presence of fungal species.
Otitis externa treatment focuses on preventing progression of the infection, and treating the precipitating problem. Swimmer’s ear can be treated fairly simply with dry ear precautions and antibiotic drops. When caught early, it can improve within 2-3 days of proper treatment and be gone within a week. Treatment can be accelerated if the otolaryngologist first cleans out the ear of discharge and debris with suction or a curette. Patients are typically discouraged from attempting to clean their own ear to avoid further irritation and/or spread of the disease. If there is no damage to the eardrum, the patient can be prescribed eardrops that may include:
- Antibiotics to treat the bacterial infection
- Antifungal agents to treat the fungal infection
- Steroids to reduce swelling
- An acidic solution to address any pH imbalance
More advanced cases of otitis externa and their complications are typically treated with intravenous antibiotics. Surgery is rarely necessary. Treatment varies based on the causative organism (i.e., fungal, bacteria, viral).
Because people who experience otitis externa once are more likely to have it again, prevention is necessary. One of the most important aspects is to have dry ears. After swimming or other water exposure, the patient should dry his/her ear with a hair dryer to avoid moisture accumulation. These patients should not insert anything into their ears to clean them, including cotton swabs, towels, soap or other similar objects. Soap can alter the normal pH balance of the ear canal.
Key Facts
- Ears should be dried shortly after exposure to water.
- Do not clean ears with cotton swabs, the ends of towels, etc; Use a hairdryer instead.
- Symptoms of otitis externa include redness, itching, fever and a feeling of fullness in the ear.
- If you suspect otitis externa, go to a doctor as soon as possible.
- Patients who have had otitis externa are at risk of repeat episodes.
To learn more about otitis externa or Dr. Ronen Nazarian, please visit: www.ohni.org.