- Hereditary Hemorrhagic Telangiectasia - May 25, 2016
- Hereditary Hemorrhagic Telangiectasia: Septal Perforation and Nose Bleeds - May 23, 2016
- Hereditary Hemorrhagic Telangiectasia: Epistaxis and Septal Perforation - May 18, 2016
- Wegener’s Granulomatosis: Autoimmune Disease and Multi-Focal Septal Perforation - May 9, 2016
- Kyle Korver: Facial Injury and Nasal Fracture - March 24, 2015
- Russell Westbrook: Facial Injury and Surgery - March 5, 2015
- Mega-perforation: Pushing the Limits of Septal Perforation Repair - November 26, 2014
- Septoplasty Complication and Septal Perforation - November 24, 2014
- Nose Picking (Rhinotillexis) and Septal Perforations: Why I should stop picking my nose…? - November 24, 2014
- Nasal Fractures, Septal Hematoma, and Septal Perforation: Simultaneous Rhinoplasty and Septal Perforation Repair - October 1, 2014
Is Frey’s Syndrome an avoidable surgical complication of parotid surgery?
Question: I recently had surgery to have my parotid gland removed. I noticed that a short time after surgery, part of my face began to sweat when I would eat and sometimes even shortly before eating. I also noticed flushing over the same part of my face and neck. My physician believes that this “gustatory sweating” may be due to Frey’s Syndrome. Could Frey’s Syndrome have been avoided?
Discussion:
Frey’s Syndrome is a common, yet avoidable, surgical complication that is due to trauma of a specific structure, the auriculotemporal nerve. The auriculotemporal nerve controls salivation by signaling the parotid gland to secrete saliva. Traditional surgery of the parotid gland typically damages the auriculotemporal nerve due to the extensive dissection of the parotid gland and surrounding areas of the face. When the nerve regenerates it attaches to the skin abnormally because the parotid gland has been removed, causing Frey’s Syndrome. Advanced surgical techniques which minimize the damage to these delicate areas decrease the likelihood of developing Frey’s Syndrome. In addition to minimizing surgical trauma, proper facial reconstruction of the resulting parotid defect is key to preventing Frey’s Syndrome as well as undesirable cosmetic changes left by traditional parotid gland interventions. Reconstructive procedures performed during your parotid surgery, provide a physical barrier between the auriculotemporal nerve and sweat gland structures thereby preventing abnormal facial sweating while eating (gustatory sweating) and flushing. This barrier, which is typically grafted from your own skin, also restores a natural sense of facial symmetry which is often times impacted by the defect seen in parotid surgery. Late reconstruction is also an option for patients with Frey’s syndrome from a previous surgery.
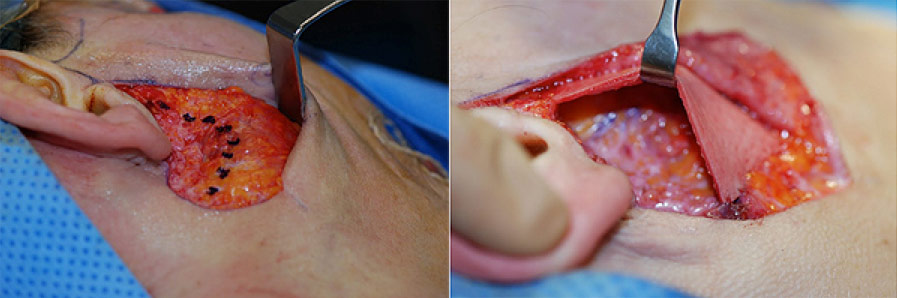
Drs. Ryan Osborne and Jason Hamilton of the Osborne Head and Neck Institute have pioneered the use of minimally invasive surgical techniques for treating disorders of the parotid gland, namely, the mini‑incision method. The mini-incision method safeguards the integrity of the auriculotemporal nerve as well as the facial nerve by decreasing the size of the incision and the resulting damage to the underlying structures of the face. Advanced techniques for treatment and reconstruction of the parotid gland are unlikely to be routinely employed in conventional settings. The Osborne Head and Neck Institute performs 3-4 parotid surgeries per week whereas a typical surgeon may perform as many as 4 procedures per year. Minimally invasive technique with reconstruction remains the gold standard for preventing and treating Frey’s Syndrome.
Key Points:
- Frey’s Syndrome is a rare, yet preventable, surgical complication of traditional parotid surgery.
- Advanced surgical techniques pioneered at the Osborne Head and Neck Institute, such as the mini-incision method, avoid complications such as Frey’s Syndrome.
- Reconstruction of the parotid defect is paramount in preventing or treating Frey’s Syndrome as well as restoring facial symmetry.
- Osborne Head and Neck Institute physicians, Ryan Osborne and Jason Hamilton preform 3-4 parotid surgeries per week using advanced techniques whereas traditional surgeons may perform at most 4 parotid surgeries per year.
For more information on Parotid surgery or treatment of Frey’s Syndrome, please contact the Osborne Head and Neck Institute.