- Folded Ear in Newborns: Treatment Options - April 11, 2018
- Newborn Ear Deformity: What Can Be Done? - April 11, 2018
- Ear Molding: An Overview - November 2, 2017
- Otoplasty for Protruding Ears - September 26, 2017
- Basal Cell Carcinoma: Facial Reconstruction Timing - September 26, 2017
- Clinical Considerations of Mohs Reconstruction of Cheek Defect - September 26, 2017
- Basal Cell Carcinoma: Nasal Bridge Reconstruction - September 26, 2017
- Skin Cancers Involving the Eyebrow: Clinical Considerations - October 3, 2016
- Treatment of Multiple Skin Cancer Lesions - June 1, 2016
- Skin Cancer: Nasal Reconstruction and Scar Management - June 1, 2016
Why should a nasal fracture be evaluated in a timely fashion?
Question: I play basketball for my school and was recently injured during a game when I caught an elbow to the face. I thought my nose had been broken because of the pain but it only seems like I have a lot of swelling, bruising, and minor difficulty breathing. I spoke to my primary care doctor over the phone and he mentioned that I should have my nose evaluated soon because I most likely have a fracture. With my busy sports schedule, I am not sure if I can make it in to see the doctor any time soon. Can my evaluation wait a few weeks or is it crucial that I be seen this week?
Discussion:
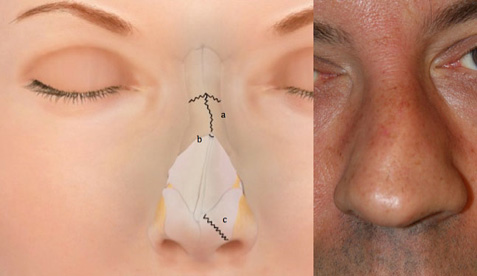
A qualified facial trauma specialist should promptly evaluate any trauma that results in a suspected nasal fracture. If a fracture is addressed within the first two weeks after injury, a physician may be able to restore or maintain the original positions of the nasal bones so that proper healing may occur. Functional concerns such as nasal obstruction and undesirable cosmetic changes can be avoided in this early treatment scenario. Conversely, if evaluation is postponed until after two weeks from the initial trauma, bone healing will have already begun and any correction to the nose’s shape or function will have to be performed surgically several months later. If evaluation is skipped altogether, possible consequences include permanent changes in breathing and cosmetic changes to the shape of the nose.
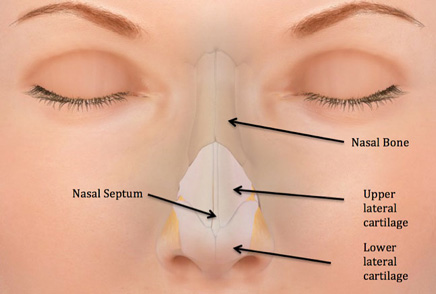
It is common for nasal fractures to go unnoticed shortly after trauma due to swelling which can camouflage resulting misalignment or bone displacements. During an early evaluation a physician will check for fractures, laceration, and damage to surrounding structures that may not be readily evident due to the effects of swelling. A CT scan or x-ray is commonly ordered to evaluate for any changes that may not be apparent from the surface and to determine the status of delicate underlying structures. A common consequence of nasal trauma, other than fracture, is the formation of a septal hematoma where blood collects within the tissues of the nasal septum that serves to divide our nose into two passages. This abnormal collection of blood can potentially block the nasal passages, making it difficult to breathe through the nose. Additionally, misalignment or perforations of the septum are also complications common to nasal trauma, which require reconstruction for proper breathing function.
There exist several options for repair of nasal fractures dependent on the timing and extent of trauma. If it is determined that the extent of the trauma is not severe and fractures have not resulted in dislocation of bone fragments, little correction is necessary and casting is usually placed to preserve the location of the nasal bones while healing takes place. In other instances where some dislocation or misalignment has taken place, the physician can realign the nose to its original position and place a cast so that healing can occur, undisturbed. Lastly, reconstructive procedures may be necessary in instances of more severe damage to the nasal bones, septum, or cartilage of the nose. Oftentimes, treatment of nasal fracture can be combined with rhinoplasty procedures to enhance or reconstruct the shape and function of the nose.
Dr. Jason Hamilton, Director of the Facial Plastic and Reconstructive Surgery Division at the Osborne Head and Neck Institute performs various nasal procedures regularly, including rhinoplasty. Dr. Hamilton is double board certified in otolaryngology and plastic and reconstructive surgery, a rare combination held by only 800 physicians worldwide. This special set of qualifications allows Dr. Hamilton to thoroughly evaluate and treat all aspects of nasal trauma.
Key Points:
- A qualified facial trauma specialist should promptly evaluate any facial trauma that results in a suspected nasal fracture.
- If a fracture is addressed within the first two weeks after injury, a physician may be able to restore or maintain the original positions of the nasal bones so that proper healing may occur.
- If evaluation is postponed until after two weeks from the initial trauma, bone healing will have already begun and any correction to the nose’s shape or function will have to be performed surgically several months later.
- It is common for nasal fractures to go unnoticed shortly after trauma due to swelling which can camouflage resulting misalignment or bone displacements.
- There exist several options for repair of nasal fractures and the complications arising from nasal trauma.
To learn more about Dr. Hootan Zandifar or nasal fracture evaluation and treatment, please visit www.facialtraumamd.com.